We found out
from the Department Health Services last week that the State of Wisconsin is forecast to have another $221 million available in GPR (basically state tax dollars) to spend over the next 15 months, on top of the $3.8 billion we were already are projected to have.
The Department projects a surplus in the Medicaid program of $406.1 million GPR for the 2021-23 biennium……[reflecting] current estimates for Medicaid expenditures through FY 23, based on trends in enrollment, costs per enrollee, federal Medicaid participation, and third party revenues.
That’s up a significant amount from the projection of a $184.9 million surplus 3 months ago so why is that? Because Omicron’s breakout meant that the Feds will continue to pay a larger share of the state’s Medicaid bill.
The primary reason for the significant increase in the projected surplus since last quarter’s update is a further extension of the federal COVID-19 public health emergency declaration. Effective January 16, 2022, US Health and Human Services Secretary Xavier Becerra extended the emergency for 90 days until April 16, 2022. The Families First Coronavirus Response Act (FFCRA) adds 6.2 percentage points to the federal Medicaid match rate for expenditures during calendar quarters in which the public health emergency is in place. With the extension issued this past January, the enhanced match rate will be in place through June 2022. Act 58, the 2021-23 biennial budget, assumed the enhanced matched rate would end in December 2021. The Medicaid program must also continue to comply with FFCRA continuous coverage requirements during the public health emergency. The net impact of additional federal revenue, offset by higher enrollment due to the continuous coverage requirements, is $95 million GPR.
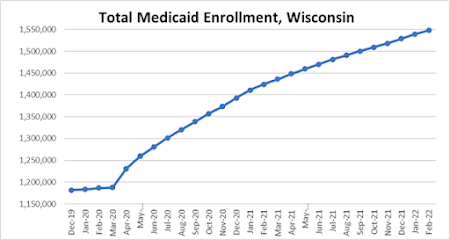
The
“continuous enrollment” requirement basically keeps people from being kicked off of Medicaid for as long as the COVID emergency continues. This explains why Medicaid enrollments have continued to grow every month and is now 30% above pre-pandemic levels, even as the state’s economy has recovered to a record-low unemployment rate.
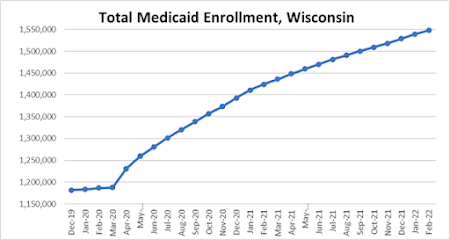
DHS anticipates that the emergency provisions will end, and that the number of people on the Medicaid rolls would drop quickly by May 2023 “to a level slightly above actual enrollment as of March 2020.” That rapid decline in enrollment accounts for $70 million of the additional Medicaid surplus, but it also would mean around 300,000 to 350,000 people wouldn’t be getting their health insurance through BadgerCare and other Medicaid programs.
Seems like something we need to keep an eye on, especially if the COVID health emergency ends in 2 weeks, which would allow Wisconsinites and many other Americans to be disenrolled off of Medicaid starting in July. And if I were in the Biden Administration, I’d say this would be a big reason not to end the health emergency this year, because who needs that disruption before the 2022 elections, especially with it being unknown what will happen in the Fall/Winter flu/COVID season?
It seems certain that the emergency declaration would be in place through at least the end of September, under guidance from last year that said
there would be 60 days notice given to states if the emergency declaration was going to end, and that hasn’t happened with less than 2 weeks left in the current declaration.
Until last week, the Wisconsin DHS also benefitted from another source of Federal help in paying for parts of Medicaid, and that’s in Home and Community Based Services (HCBS) that deals with long-term care needs and other services in settings outside of nursing homes and medical facilities. The money came from President Biden’s ARPA stimulus package and gives an extra boost from Uncle Sam in paying for these services.
….The federal ARPA legislation enables state Medicaid programs to claim an extra 10 percentage points of federal Medicaid match on eligible HCBS expenditures from April 1, 2021 through March 31, 2022. As a condition of receiving these funds, the state must reinvest an equivalent amount in a place to enhance, expand, and strengthen Medicaid HCBS. The state has until March 31, 2025 to spend the reinvestment funds, and it can draw additional federal funding for reinvestments in Medicaid-eligible activities. Because of the reinvestment requirement, the enhanced HCBS match does not result in GPR savings in the current biennium.
While there’s no GPR savings, it also means that state tax dollars aren’t being used for initiatives such as a 5% increase in rates paid to providers of HCBS services, and a 16% rate increase to ambulance providers that took effect in February. This can help staff up those services, and increase the chances of providers of all sorts to stay in the business.
The GOP-run Joint Finance Committee has had no problem with approving all of this additional Federal help to pay for Medicaid services over the last 2 years. Which begs an obvious question -
why don’t they want to have the Feds cover even more of Medicaid’s expenses by taking the expansion of services that is offered in Obamacare?
Seriously, what reason could you have after the last 2 years and the success of stability for those in need of health insurance? But the real reasons for WisGOP's continued foolishness on this issue seem to be:
1. Having the name of the Black Man in the White House associated with it, and
2, Being bought by the insurance industry and corporate oligarchs (because how dare the working poor be given insurance choices – they might look for better jobs!),
Other than that, I have no idea. But given that these COVID-related Medicaid provisions are going to end some time soon, it might be worth it for Governor Evers and other Dems to point out that we've already had expanded Medicaid funding in this state for the whole COVID era, and it's worked pretty well. So why not take the last step and save hundreds of millions of state tax dollars by permanently expanding Medicaid?
No comments:
Post a Comment